You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
With a 5.6% increase in 2016, healthcare is the fastest growing sector of the US economy, comprising 17.8% ($3.22 trillion in 2015) of the gross domestic product. The Centers for Disease Control and Prevention (CDC) estimated that 18 million people are working in the US healthcare industry and related occupations (eg, employees, employers, students, contractors, public safety workers, and volunteers), and more than 900,000 are dental healthcare workers. Women represent nearly 80% of the current healthcare workforce.1-4
Healthcare workers (HCWs) face many noninfectious occupational hazards. Examples include hazardous chemicals, latex allergies, lasers, radiation, stress, violence, strains, sprains, and heat/fire. Also, HCWs are exposed to infectious agents, including bloodborne pathogens, such as hepatitis B virus (HBV), hepatitis C virus (HCV), and human immunodeficiency virus (HIV). Occupational exposure to patient blood and other body fluids poses a serious public health concern.1,5
Healthcare Personnel and Occupational Exposures
Many HCWs are at risk for infectious occupational hazards. Exposure can involve: (1) percutaneous injuries with a contaminated sharp object (eg, needles, blades, pointed instruments, and broken glass); (2) direct contact (ie, contact without barrier protection) and inhalation (via non-intact skin and mucous membranes); and (3) contaminated environment surfaces (eg, fomites) or instruments/equipment (ie, indirect contact). The number of nonfatal HCW occupational injuries and illnesses is the highest among any industry sector.1,3,5,6
The risk of bloodborne pathogen transmission is dependent on the prevalence of HBV, HCV, and HIV in the American population, the environmental survival of the bloodborne pathogens, and their transmissibility via percutaneous, mucous membrane, or intact skin exposure.1,5,6
Hepatitis B Virus
The seroprevalence of persons with active cases of HBV in the general population is approximately 0.4%. HBV can survive and remain infectious outside source patients for 7 days or longer. HBV DNA can be detected on environmental surfaces in the absence of visible blood.1,5
HBV is primarily transmitted by percutaneous or mucosal exposure. Efficiency of HBV transmission depends on viral load, route of transmission, and the immune status of the HCW affected. A generalized estimate of transmission after a percutaneous injury (used hollow needle, not a solid instrument) is 33% (1 in 3) for HBV. Most HCW infections occurred before widespread vaccination began. In 1983, there were 10,000 occupationally acquired HCW cases. However, in 2002, there were fewer than 400. Hepatitis B vaccination is the most effective measure to prevent HBV infections. Immunization provides both pre- and post-exposure protection against HBV infection.1,5,6
Because of possible high viral loads and an ability to remain stable at ambient temperatures, HBV transmission also can occur after exposure to environmental surfaces or equipment that have been unsuccessfully disinfected.1,5
The need for post-exposure prophylaxis (PEP) after accidental percutaneous or mucosal exposure to blood depends on several factors. These include the hepatitis surface antigen status of the source patient (measure of infectivity), completion of the hepatitis B vaccination series, and vaccine response of the exposed HCW. Prophylaxis, if needed, should include prompt start of hepatitis B vaccination and injection of hepatitis B immune globulin.1,5
Hepatitis C Virus
HCV is the most common chronic bloodborne infection in the United States, affecting an estimated 2.7 million to 3.2 million people. An estimated 30,500 acute hepatitis C cases occurred in 2014. The seroprevalence of persons capable of infecting others of HCV in the general population is approximately 1.3%.1,5,7
Environmental survival of bloodborne pathogens varies. HCV degrades at room temperatures even if within serum. Studies place HCV environmental survival between 16 hours and a maximum of 4 days. The potential for environmental survival and the possible presence of HCV-contaminated blood environmentally allows for the potential risk of transmission in healthcare settings.1,5,7
HCV transmission occurs primarily through exposure to infected blood. A generalized estimate after a percutaneous injury (used hollow needle, not a solid instrument) is 1.8% (1 in 55). Transmission from mucous membrane exposure to blood rarely occurs, and it happens even less frequently with exposure of non-intact skin. HCV is not known to be transmitted through airborne or causal contact.1,5,7
No vaccine exists to prevent HCV infection. Protection centers on limiting exposure to infectious blood. Currently, there is no PEP for HCV.5
Human Immunodeficiency Virus
The primary means for acquiring HIV among adults is the exchange of body fluids. Perinatal transmission also is possible. HIV is not transmitted by airborne routes, household or workplace contact, exposure to contaminated environmental surface, or insect vectors. HIV is readily inactivated by most common disinfectants, including diluted household bleach (1:10 to 1:100).1,5
A generalized estimate for HIV after a percutaneous injury (used hollow needle, not a solid instrument) is 0.3% (1 in 333).1,5,8,9 The environmental half-life for HIV is 28 hours with a potential maximum of several days.1HIV acquisition by mucous membrane routes is 0.09% (1 in 1111) and by contact with non-intact skin is probably less than 0.1% (1 in 1000); however, this has not been completely quantified.1,5
HCWs sustaining accidental parenteral exposures must immediately clean the site with soap and water and seek immediate medical care. Mucous membrane exposures require liquid rinses. Exposed HCWs need baseline and regular follow-up counseling for 6 months (eg, at 6 weeks, 3 months, and 6 months) to diagnose infection development.
Preventing occupational exposure is the most important strategy for reducing the risk for occupational acquisition of HIV infection. However, if possible, there should also be a PEP plan. This includes whether the exposed person should receive PEP (antiretroviral medication taken as soon as possible after exposure to reduce the chance of HIV infection) and what type of PEP regimen is needed. For most HIV exposures that warrant PEP, a 4-week, two-drug regimen is recommended, starting as soon as possible after exposure (within 72 hours). If there is an increased risk of transmission (based on the viral load of the source and the type of exposure), a three-drug regimen is recommended. Other specific recommendations may apply if there is a delay in exposure reporting, the source is unknown, the exposed person is pregnant, there is resistance of the source virus to antiretroviral agents, or there is toxicity of PEP regimens.1 The US Public Health Service recommends post-exposure chemoprophylaxis with antiretroviral agents for needlesticks from HIV-infected sources and mucous membrane and non-intact skin exposures to such sources.1,5,8
Sharps Injuries
CDC estimates that about 385,000 sharps-related injuries (penetrating stab or puncture wound) occur annually among HCWs in hospitals. It is estimated that about at least half of sharps injuries go unreported. Most sharps injuries involve nurses; however, laboratory staff, physicians, housekeepers, and other HCWs also can be injured.7,8
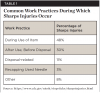
In addition to the use of sharps devices, injuries are also closely associated with certain work practices that can pose an increased risk of bloodborne pathogen exposure. Common work practices include disposal-related activities; activities after use and prior to disposal, such as item disassembly; and recapping a used needle (Table 1).7-9
Also, injuries are closely associated with certain devices that can pose an increased risk of bloodborne pathogen exposure. These devices include disposable syringes, suture needles, and other types of sharps (Table 2).8,9
Considering the frequency of their exposure to blood and other body fluids, the number of HCWs in the United States infected with HIV through occupational exposure is quite small.1,5,8,10 The greatest HIV risk follows a percutaneous injury involving a contaminated sharp, especially a hollow needle that has been in the vein or artery of an HIV-positive source patient. Risk increases for patients with Stage 3 HIV infection (ie, acquired immunodeficiency syndrome [AIDS]), as high viral loads are often involved this late in the disease process.1,3,9,10
In the United States, 58 confirmed cases and 150 possible cases of occupationally acquired HIV infection were reported to the CDC between 1985 and 2013 (Table 3). Since 1999, however, only one confirmed case (a laboratory technician who sustained a needle puncture while working with a live HIV culture in 2008) has been reported (Table 4). Of course, underreporting is a possibility because reporting is voluntary.1,9,10
A confirmed case of occupationally acquired HIV infection requires documentation that seroconversion in the exposed HCW is temporally related to a specific exposure to a known HIV-positive source. A possible case of occupationally acquired HIV infection is defined as an infection in a HCW whose job duties might have exposed him or her, but who lacks a documented workplace exposure. The HIV status of a source patient may be unknown or the HCW seroconversion after exposure may not have been documented as temporally related. Thus, occupational acquisition of HIV infection is possible without it being confirmed.3,10,11
Among the 58 confirmed cases, the routes of exposure resulting in infection were percutaneous punctures or cuts (49 cases), mucocutaneous exposures (5), both percutaneous and mucocutaneous exposures (2), and unknown (2). A total of 49 HCWs were exposed to HIV-infected blood, four to concentrated virus in a laboratory, one to visibly bloody fluids, and four to unspecified body fluids.3,10,11
Standard Precautions
CDC recommends the use of standard precautions to prevent exposure of HCWs to potentially infectious body fluids when working with any patient, whether he or she is known to be infected with HIV or not. This means that HCWs should assume that all patient body fluids are potentially infectious.1,5,10Properly implemented standard precautions include the use of safety devices and barriers such as gloves and protective eyewear to minimize exposure risk.1,5,10
To prevent puncture injuries, CDC recommends a comprehensive prevention program consistent with requirements of the Occupational Safety and Health Administration's Bloodborne Pathogens Standard.12 This includes use of medical devices engineered for sharps protection (eg, needleless, self-sheathing systems). Used devices such as syringes or other sharp instruments should be disposed of in sharps containers without attempting to recap needles. While many factors come into play, safer work practices help reduce the chances of occupational HIV exposure and result in lower numbers of infections.
HIV Cases Dropping
In 2015, 39,513 people were diagnosed with HIV infection in the United States. The number of new HIV diagnoses fell 19% from 2005 to 2014. Because HIV testing has remained stable or slightly increased in recent years, this decrease in diagnoses suggests a genuine decline in new infections. The decrease may be due to targeted HIV prevention efforts. However, progress has been uneven and diagnoses have increased among a few groups.10,13,14
At the end of 2014, the most recent year for which such data are available as of this writing, an estimated 1,107,700 adults and adolescents were living with HIV with an estimated 166,000 (15%) remaining undiagnosed. Young people were the most likely to be unaware of their infection. Among people aged 13 to 24, an estimated 51% (31,300) of those living with HIV at the end of 2013 did not know it.3,10-12
Worldwide, the number of newly diagnosed cases of HIV dropped about 33% (3.4 million to 2.3 million) from 2001 to 2013. Also, potent antiretroviral therapy has significantly increased longevity among HIV-infected patients. As this patient population grows older, an increased need for surgical interventions, such as coronary revascularization, will likely rise. Concerns about HIV-positive patients who need surgery include morbidity and mortality, preoperative evaluation, and post-surgical management. It is estimated that 25% of these individuals will need surgical/anesthesia treatment during their illness.10,13,14
Conclusion
Healthcare workers, including dental personnel, are constantly at risk for both noninfectious and infectious occupational hazards, and the risk of bloodborne pathogen transmission is quite prevalent. Occupational exposure to patient blood and other body fluids poses a serious health concern, and proper care must be emphasized to prevent occupational acquisition of bloodborne pathogens.
About the Author
Charles John Palenik, MS, PhD, MBA
President and CEO, GC Infection Prevention and Control Consultants, Indianapolis, Indiana. In 2011, Dr. Palenik retired after 35 years at Indiana University School of Dentistry, where he held a number of academic and administrative positions, including Professor of Oral Microbiology, Director/Human Health & Safety, Director/Central Sterilization Services, and Chairman/Infection Control and Hazardous Materials Management Committees.
Queries to the author regarding this course may be submitted toauthorqueries@aegiscomm.com.
References
1. Weber DJ, Rutala WA. Occupational health update: focus on preventing the acquisition of infections with pre-exposure prophylaxis and postexposure prophylaxis. Infect Dis Clin North Am. 2016;30(3):729-757.
2. Drum K. Chart of the day: health care spending as a percentage of GDP. Mother Jones website. June 5, 2017. http://www.motherjones.com/kevin-drum/2017/06/chart-day-health-care-spending-percentage-gdp/. Accessed August 1, 2017.
3. National Institute for Occupational Safety and Health. Healthcare workers. Centers for Disease Control and Prevention website. Updated March 14, 2017. http://www.cdc.gov/niosh/topics/healthcare/. Accessed August 1, 2017.
4. Solomon ES. The past and future evolution of the dental workforce team. J Dent Educ. 2012;76(8):1028-1035.
5. Miller S. Occupational exposure to bloodborne pathogens. In: Grota P, ed. APIC Text of Infection Control and Epidemiology. Washington, DC: Association for Professionals in Infection Control and Epidemiology; 2014.
6. National Institute for Occupational Safety and Health. Bloodborne infectious diseases: HIV/AIDS, hepatitis B, hepatitis C. Centers for Disease Control and Prevention website. Updated April 5, 2017. https://www.cdc.gov/niosh/topics/bbp/default.html. Accessed August 1, 2017.
7. Centers for Disease Control and Prevention. Hepatitis C FAQs for health professionals. Centers for Disease Control and Prevention website. Updated January 27, 2017. https://www.cdc.gov/hepatitis/hcv/hcvfaq.htm#section. Accessed August 1, 2017.
8. Centers for Disease Control and Prevention. Occupational HIV transmission and prevention among health care workers. Centers for Disease Control and Prevention website. Updated November 7, 2016. https://www.cdc.gov/hiv/workplace/healthcareworkers.html. Accessed August 1, 2017.
9. National Institute for Occupational Safety and Health. Stop sticks campaign. Centers for Disease Control and Prevention website. Updated June 24, 2011. https://www.cdc.gov/niosh/stopsticks/sharpsinjuries.html. Accessed August 1, 2017.
10. Joyce MP, Kuhar D, Brooks JT. Notes from the field: occupationally acquired HIV infection among health care workers - Unites States, 1985-2013. MMWR Morb Mortal Wkly Rep. 2015;63(53):1245-1246.
11. Centers for Disease Control and Prevention. HIV in the United States: at a glance. Centers for Disease Control and Prevention website. Updated June 9, 2017. https://www.cdc.gov/hiv/statistics/overview/ataglance.html. Accessed August 1, 2017.
12. OSHA Fact Sheet. OSHA's Bloodborne Pathogens Standard. Occupational Safety and Health Administration. https://www.osha.gov/OshDoc/data_BloodborneFacts/bbfact01.pdf. Accessed August 1, 2017.
13. Wyzgowski P, Rosiek A, Grzela T, Leksowski K. Occupational HIV risk for health care workers: risk factor and the risk of infection in the course of professional activities. Ther Clin Risk Manag. 2016;12:989-994.
14. Prout J, Agarwal B. Anaesthesia and critical care for patients with HIV infection. Continuing Education in Anaesthesia, Critical Care & Pain. 2005;5(5):153-156.