You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
Managing pain after dental surgical procedures is vital for bringing positive energy to a patient, both physically and mentally, for the duration of the physiologic healing process. Knowing a patient's personality and expectations after surgical procedures is critical for the clinician in regard to patient compliance, medication safety (risk and benefits), and appropriateness of a medication for the expected pain level and the patient's lifestyle.
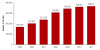
Based largely on the increase in drug abuse with opioids such as Vicodin (acetaminophen/hydrocodone) and Percocet (acetaminophen/oxycodone), the number of visits to the emergency department (ED) in recent years has increased substantially. Lifestyle habits of patients combining alcohol and opioids have also contributed to the increase. Figure 1, Figure 2, and Table 1 show how drug combinations have contributed to narcotic pain reliever-related ED visits involving nonmedical use of pharmaceuticals.1,2 Dentists should consider the optimum benefits for alternatives to opioid prescription medications for managing acute postoperative dental pain. Alternatives are safer for the patient and protect the dentist medically and legally from potential litigation for inappropriate prescription writing regarding pain management.3
This article will discuss the effects of opioid medications on mu and kappa receptors, the conversion of opioids to the morphine form, opioid side effects, and opioid toxicity. After this discussion, alternative non-opioid prescription medications for managing acute dental pain will be presented, along with basic regimens of non-steroidal anti-inflammatory drug (NSAID) and acetaminophen combination therapy. Additionally, alternative medications (prednisone) (Table 2) (eg, glucocorticosteroids),4 local anesthetic administration for postsurgical pain management, and the logic behind the multimodal approach will be discussed.
Opioid Considerations
Management of acute pain after dental procedures involving nerves, soft-tissue manipulation, extractions, and osseous reduction has been covered in medical literature for many years. However, statistical data for utilization of opioids within dentistry and the effects of opioids on pain management suggest that alternative non-opioid medications, corticosteroids, NSAIDs, and local anesthetics postoperatively are more appropriate.5-7 After surgical or endodontic procedures, patients will undergo the process of fighting inflammation of soft-tissue or perineural structures. Inflammation can also result from a localized physical condition in which part of the body becomes reddened, swollen, hot, and often painful, especially as a reaction to injury or infection.5 Dentists must accurately diagnose, treat or not treat, and when necessary, prescribe the appropriate medications to resolve the inflammation from the procedure, injury, or infection.
Opioids are often prescribed to handle pain after dentistry procedures. They are similar to endorphins. Endorphins and opioids have two receptors, mu and kappa. The effects of opioids are similar on receptors, producing analgesia, respiratory depression, sedation, and miosis. The receptors differ slightly in opioid effects by creating feelings of euphoria or dysphoria. Mu receptors have a propensity for euphoria dependence; consequently, opioids can lead to physical and psychological addiction.8 Because opioids stimulate the parts of the brain that are connected to reward, some users experience a "high" feeling when they take even legitimately prescribed doses of these medications. This feeling of euphoria can cause addiction to opioid narcotics.8 Concurrently, in regard to kappa receptors, opioids can lead to the development of dysphoria, a behavior or a state of feeling very unhappy, uneasy, or dissatisfied.8 The situation presents a patient management issue and should be discussed with the patient before an opioid prescription is written when the decision has been made to prescribe an opioid to manage acute pain.9
Opioids have unlimited efficacy, and equipotent doses are equal in pain relief.8 However, orally administered opioids are limited by the process of first-pass metabolism. First-pass metabolism is a process in which a drug administered by mouth is absorbed from the gastrointestinal tract and transported by the portal vein to the liver, where it is metabolized. As a result, in some cases only a small proportion of the active drug reaches the systemic circulation and its intended target.
Another consideration is an enzyme responsible for converting opioids into morphine form, through demethylation: CYP-2D6. CYP-2D6 is an important detoxifying enzyme responsible for the clearance of 20% of clinical drugs, including opioids (codeine, tramadol), antitumor drugs (tamoxifen), antidepressants (fluoxetine), and antipsychotics (haloperidol).10 This enzyme also metabolizes dopamine and serotonin. As an example, after a patient who is not taking any additional medication swallows a codeine tablet, first-pass metabolism begins; after this process, only 60% of the oral dose of codeine is bioavailable.10 The remaining drug may cause nausea and vomiting as well as constipation.10 Continuing with another example, a patient may be taking additional medications such as cimetidine, fluoxetine, and paroxetine. These medications inhibit the ability of the hepatic enzyme CYP-2D6 to demethylate the codeine to the active morphine form.8 The patient will most likely not benefit from a codeine prescription or any other opioid prescription.11
As life expectancy of the population increases, dentists will see more geriatric patients in their offices. Geriatric patients most likely will be taking multiple medications and be in need of pain management for dental procedures, injuries, or infections. In regard to prescribing opioids, geriatric patients are more sensitive to central nervous system effects and decreased renal and liver functions. Due to these sensitivities, dentists should consider a reduction in dosage by one half the usual dose or avoid using opioid prescriptions completely.8 NSAIDs for geriatric pain management have both anti-inflammatory and analgesic properties; thus, their use in dentistry is advantageous. NSAIDs are widely used by the geriatric population because of the high prevalence of chronically painful conditions, such as arthritis. In cases of dental pain, several NSAIDs have been shown to be effective, including ibuprofen, naproxen, flurbiprofen, diflunisal, and ketorolac.8 However, NSAIDs are associated with some adverse effects, the most concerning of which is their effect on the gastrointestinal tract. NSAIDs can cause gastric erosion, which can lead to ulcers and then gastric bleeding. In the elderly, these effects tend to be more severe than in younger people.12
Opioid Allergy vs Pseudo-Allergy
Sometimes patients will state that they are allergic or have had an allergic reaction to opioids. The clinician should question the patient's statement regarding the symptoms that arose after oral administration of the opioid. Was there nausea and vomiting or pruritus? Itching after taking opioids may have been a result of morphine-induced histamine release after first-pass metabolism.13 A patient who experiences an allergic or pseudo-allergic reaction may need to undergo allergy testing and avoid opioids completely. Growing evidence shows that numerous drug-induced allergies are not mediated by the pathogenic role of the allergen-specific immunoglobulin E (IgE).14 Pseudo-allergy (non-IgE mediated) mechanism is based on mast-cell basophil activation. The symptoms resemble true allergy but are caused by histamine release from cutaneous mast cells. Patients who exhibit these reactions should be prescribed corticosteroids or NSAIDs.13 Published data suggest that 9 out of 10 patients labeled with an opioid allergy do not have a true opioid allergy.15 However, when a patient truly presents with an opioid allergy and the nature or cause is unclear, all opioids should be withheld.8 A thorough review of the patient's medical history can assist in choosing a safer medication. Symptoms, diet, and other medications the patient may have taken before the allergic reaction should be evaluated. Elevated IgE levels suggest a true allergy, but IgE could also be elevated for reasons unrelated to opioid allergy.9,15
Opioid Toxicity
Symptoms of opioid toxicity include confusion, agitation, visual defects, vivid dreams or nightmares, and visual/auditory hallucinations. Opioid toxicity can be managed by giving adequate hydration, acutely treating agitation, reducing dosage, or switching to a different opioid.14
Opioids and Respiratory Depression
As opioid dosage is increased, the respiratory center may become less sensitive to carbon monoxide, resulting in respiratory depression.16 Decreases in respiratory rate are often preceded by severe sedation. Risk of respiratory depression is increased by excessive dose of opioids greater than needed to relieve pain or doses given/taken when no pain is present. Opioids are prescribed and titrated against the pain that is present in order to keep respiratory depression at a minimum. Pure narcotic antagonists such as naloxone reverse respiratory depression. When opioid doses increase, severe sedation increases and respiration decreases. These warning signs suggest the dosage should be reduced.17 Opioid sedation is common in the first few days of opioid administration and after subsequent dose increases, but it often resolves quickly.8
Alternative Non-Opioid Medications
NSAIDs are an alternative for pain management within dentistry. Other alternatives include glucocorticosteroids and local anesthetic after dental therapies and painful events from injury or infection. These alternatives most often are more appropriate medications than opioids for managing acute pain.7,18
NSAIDs
Aspirin and related NSAIDs impede cyclooxygenase (COX) activity at the site of tissue injury. Besides inhibiting inflammation, fever, and pain, aspirin and other NSAIDs also impede arachidonic acid conversion to cytoprotective prostaglandins.19 Therefore, care must be taken when prescribing NSAIDs to these patients. They can lead to gastroduodenopathy that delay healing; additionally, increased risk of cardiovascular episodes and prolonged bleeding may occur.20 Maximum recommended dose (MRD) for ibuprofen is 3,200 mg per day (800 mg every 6 hours); naproxen MRD is 1,250 mg on the first day, then 1,000 mg (250 mg + 500 mg first dose, then two 500 mg every 12 hours), and a salicylic acid derivative diflunisal (MRD 1,500 mg per day) 500 mg every 12 hours.21,22 Ibuprofen has been evaluated in many clinical trials; consequently, a large amount of data are available regarding its analgesic efficacy. In general, there is no difference in analgesic responses to ibuprofen between male and female patients when managing postoperative pain.23 Meta-analyses indicate that ibuprofen produces greater analgesia than paracetamol/codeine combinations.23 Another meta-analysis of ibuprofen indicated that it produced a dose-related analgesia over the range from 200 to 800 mg.24
Glucocorticosteroids
Glucocorticosteroids, or glucocorticoids, act to reduce inflammation by inhibiting the production of multiple cells and factors involved in the inflammatory response, as well as by decreasing vasoactive and chemo-attractive factors, secretion of lipolytic and proteolytic enzymes, extravasation of leukocytes to areas of tissue injury, and fibrosis.25 Glucocorticoids also act against the immune response by inhibiting cytokine production.26 The multiple sites of action of glucocorticoids have been proposed as the reason for their greater anti-inflammatory and, possibly, greater analgesic effects than NSAIDs, which typically are more selective and only act on one site.27,28 Glucocorticoids have been shown to be very effective in reducing the periapical inflammatory response after endodontic treatment,5,29 and studies have shown anti-inflammatory effects in untreated irreversible pulpitis.30 They have also been shown to reduce bradykinin levels and postoperative pain and edema in the oral surgery third molar extraction model used in many pain studies.27 Examples of glucocorticosteroids are summarized in Table 2.
Acetaminophen
In general, acetaminophen is considered to be a very safe medication due to its low incidence of cardiovascular, gastrointestinal, renal, and bleeding events compared with NSAIDs. However, liver injury resulting from administration of acetaminophen remains a significant health concern.31 Consequently, an FDA advisory committee suggested new labeling and dosing guidelines. The statement for labeling was updated in 2015, specifying warnings of severe liver damage for those patients taking more than 4,000 mg of acetaminophen daily, with other drugs containing acetaminophen, and with three or more alcoholic beverages per day.6 This update led to the FDA mandate for reduction of acetaminophen combination drugs to 325 mg per capsule or tablet.6 Acetaminophen has analgesic effects, antifever effects, and low gastrointestinal toxicity. However, it is a weak anti-inflammatory medication.32
NSAID and Acetaminophen Combination Therapy
Research has demonstrated that ibuprofen has greater analgesic effects than aspirin or acetaminophen.33 The half-life of ibuprofen is approximately 3 hours. The maximum daily dose of ibuprofen is 3,200 mg; acetaminophen maximum dose is 4,000 mg. A combination of ibuprofen and acetaminophen is an acceptable regimen of NSAID and acetaminophen. A maximum anti-inflammatory and analgesic action requires higher doses of ibuprofen. The maximum dose should be administered every 6 to 8 hours. Acetaminophen has similar first-order pharmacokinetics and has a half-life of 3 hours as well. Acetaminophen should be administered every 6 to 8 hours in an alternating schedule from the ibuprofen schedule. The example regimen that follows was calculated by the author for avoiding taking maximum daily doses and receiving optimum pain relief in relation to understanding half-lives of both medications: The first dose of 800 mg ibuprofen can start at 8:00 am, followed by 1,000 mg of acetaminophen at 12:00 noon. Then the patient should alternate with this regimen for the entire day, alternating the ibuprofen and acetaminophen every 4 hours. The maximum daily dose of ibuprofen is 3,200 mg and maximum daily dose for acetaminophen is 4,000 mg. If one were to calculate the total mg doses of each medication based on this regimen, the patient would administer only 2,400 mg of ibuprofen and 3,000 mg of acetaminophen in a 24-hour period. Thus, both drugs do not reach the maximum daily doses.
Postoperative Local Anesthetic
Pain in the postoperative setting is an unwanted side effect of surgery directed to improve morbidity or mortality. The potential benefits of optimal postoperative pain control include improved cardiac, respiratory, and gastrointestinal functions; fewer complications; and reduced chronic postsurgical pain. Opioids have been the cornerstone of relief for perioperative pain; however, opioids have numerous side effects, including nausea, vomiting, respiratory depression, prolonged ileus, itching, tolerance, and development of opiate-induced hyperalgesia.34
The development of new long-acting local anesthetics, such as liposomal bupivacaine, is potentially important in the management of perioperative pain. Liposomal bupivacaine was granted FDA approval in 2011 and is indicated for postsurgical analgesia with a single-dose local administration to the surgical site after a procedure.35 Liposomal bupivacaine is provided as a 13.3-mg/mL solution in either a 20-mL vial (total bupivacaine, 266 mg) or a 10-mL vial (total bupivacaine, 133 mg). Approximately 3% of the total bupivacaine included in each vial is free bupivacaine, with the remainder encapsulated into the multi-vesicular liposomes that comprise DepoFoam delivery technology.18 Each liposome is made up of multiple drug-containing vesicles, each of which is surrounded by a lipid bilayer. This prolonged-release technology allows localized release of bupivacaine over several days after a single administration, resulting in a bimodal plasma concentration-versus-time curve, with a peak about 1 hour after administration (representing free extra-liposomal bupivacaine), followed by a gradual rise to a second peak about 12 to 36 hours later (representing gradual release of liposomal bupivacaine). The concentration of bupivacaine decreases slowly and is detectable for up to 72 to 96 hours, depending on the site of administration.7
Conclusion
Pain that leads a patient to seek dental advice or treatment may be a result of many different diseases or conditions of the dental, oral, facial, or nearby structures. Dental-related pain may also occur after treatment by a dentist. Therefore, dentists must be able to diagnose the source and nature of the pain, and they must be familiar with strategies for the management of dental, oral, facial, and postoperative pain. The first, and most important, step for managing pain is to diagnose the disease or condition causing the pain and identify what has caused that disease or condition.
After the diagnosis, the patient usually receives an endodontic or dental surgical procedure requiring soft- and hard-tissue manipulations. Patients have been accustomed to an understanding that they will receive opioid medications after these therapies. However, opioids are not the appropriate medications to manage postoperative pain. NSAID-acetaminophen combination regimens are most effective to manage pain. When a more significant inflammatory event presents, an addition of a glucocorticosteroid medication prescribed for 5 days is an appropriate consideration to help combat the inflammation. Fighting inflammation and providing analgesia are the elements dentists find most challenging. Opioids do not provide an adequate anti-inflammatory punch. In more severe cases of dental surgery, one may find the multimodal therapy of NSAIDs, acetaminophen, glucocorticosteroids, and liposomal bupivacaine as more effective and safer than opioid prescription therapy. NSAID-acetaminophen combination therapy and the multimodal approach have fewer side effects such as respiratory depression, nausea/vomiting, dizziness, confusion, dysphoria, and dependence euphoria.
About the Author
Thomas M. Bilski, DDS
Private Practice, Independence, Ohio
Co-Director, The Midwest Implant Institute, Columbus, Ohio
References
1. Crane EH. The CBHSQ Report: Emergency Department Visits Involving Narcotic Pain Relievers. Rockville, MD: Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality; 2015.
2. Drug Abuse Warning Network, 2011: National Estimates of Drug-Related Emergency Department Visits. Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality; 2013.
3. Risk Management: A Practical Guide for Dentists. Dentists Benefits Insurance Company. https://dentistsbenefits.com/wp-content/uploads/DBIC_risk_management.pdf. Accessed April 3, 2018.
4. Goodchild JH, Donaldson M. Treating nociceptive orofacial pain. Inside Dentistry. 2017;13(10):61-67.
5. Holland GR. Steroids reduce the periapical inflammatory and neural changes after pulpectomy. J Endod. 1996;22(9):455-458.
6. Acetaminophen prescription combination drug products with more than 325 mg: FDA statement-recommendation to discontinue prescribing and dispensing. https://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm381650.htm. Accessed February 2017.
7. Bergese SD, Ramamoorthy S, Patou G, et al. Efficacy profile of liposome bupivacaine, a novel formulation of bupivacaine for postsurgical analgesia. J Pain Res. 2012;5:107-116.
8. Interview. James L. Rutkowski, DMD, PhD. 2018.
9. Sachs CJ. Oral analgesics for acute nonspecific pain. Am Fam Physician. 2005;71(5):913-918.
10. Cohen J. All about the CYP2D6 enzyme and how it affects your brain. SelfHacked. https://www.selfhacked.com/blog/cyp2d6/. Accessed April 3, 2018.
11. Abramowicz M, Rizack MA, et al. Med Lett. 1999;41(1056):61-62.
12. Ogbru O. Nonsteroidal anti-inflammatory drugs (NSAIDs) and ulcers. MedicineNet. https://www.medicinenet.com/nonsteroidal_anti-inflammatory_drugs_and_ulcers/article.htm. Accessed April 4, 2018.
13. Saljoughian M. Opioids: allergy vs. pseudoallergy. US Pharm. 2006;7:HS-5-HS-9.
14. Nasser SM, Ewan PW. Opiate sensitivity: clinical characteristics and the role of skin prick testing. Clin Exp Allergy. 2001;31(7):1014-1020.
15. Opioid allergies… Why are most alerts wrong? Drugs & Therapy Bulletin. University of Florida. 2004;18(3):4.
16. Hill EF. Carbon dioxide depression of respiration. Br J Anaesth. 1955;27(4):196-197.
17. Otis JA, Fudin J. Use of long-acting opioids for the management of chronic pain. US Pharm. 2005;30(3 suppl):1-14.
18. Chahar P, Cummings KC III. Liposomal bupivacaine: a review of a new bupivacaine formulation. J Pain Res. 2012;5:257-264.
19. Ricciotti E, FitzGerald GA. Prostaglandins and inflammation. Arterioscler Thromb Vasc Biol. 2011;31(5):986-1000.
20. Shanmugam VK, Couch KS, McNish S, Amdur RL. Relationship between opioid treatment and rate of healing in chronic wounds. Wound Repair Regen. 2017;25(1):120-130.
21. Ibuprofen dosage. Drugs.com. https://www.drugs.com/dosage/ibuprofen.html. Accessed April 4, 2018.
22. Naproxen (oral route) proper use. Mayo Clinic. https://www.mayoclinic.org/drugs-supplements/naproxen-oral-route/proper-use/drg-20069820. Accessed April 4, 2018.
23. Averbuch M, Katzper M. A search for sex differences in response to analgesia. Arch Intern Med. 2000;160(22):3424-3428.
24. Oxford League Table of Analgesic Efficacy. http://www.jr2.ox.ac.uk/bandolier/booth/painpag/Acutrev/Analgesics/lftab.html. Accessed November 2005.
25. Pharmacology of the adrenal cortex. In: Hilal-Dandan R, Brunton LL, eds. Goodman and Gilman's Manual of Pharmacology and Therapeutics. 2nd ed. https://hemonc.mhmedical.com/content.aspx?bookid=1810§ionid=124494572. Accessed April 4, 2018.
26. Coutinho AE, Chapman KE. The anti-inflammatory and immunosuppressive effects of glucocorticoids, recent developments and mechanistic insights. Mol Cell Endocrinol. 2011;335(1):2-13.
27. Marshall JG. Consideration of steroids for endodontic pain. Endod Topics. 2002;3:41-51.
28. Becker DE. Basic and clinical pharmacology of glucocorticosteroids. Anesth Prog. 2013;60(1):25-31.
29. Smith RG, Patterson SS, El-Kafrawy AH. Histologic study of the effects of hydrocortisone on the apical periodontium of dogs. J Endod. 1976;2(12):376-380.
30. Isett J, Reader A, Gallatin E, et al. Effect of intraosseous injection of depo-medrol on pulpal concentrations of PGE2 and IL-8 in untreated irreversible pulpitis. J Endod. 2003;29(4):268-271.
31. Acetaminophen Overdose and Liver Injury - Background and Options for Reducing Injury. FDA. https://www.fda.gov/ohrms/dockets/ac/09/briefing/2009-4429b1-01-FDA.pdf. Accessed April 4, 2018.
32. 10 things you should know about common pain relievers. Harvard Health Publishing https://www.health.harvard.edu/pain/12-things-you-should-know-about-pain-relievers. Published January 2015. Updated August 16, 2017. Accessed April 4, 2018.
33. Ong CKS, Lirk P, Tan CH, Seymour RA. An evidence-based update on nonsteroidal anti-inflammatory drugs. Clin Med Res. 2007;5(1):19-34.
34. Hayhurst CJ, Durieux ME. Differential opioid tolerance and opioid-induced hyperalgesia: a clinical reality. Anesthesiology. 2016;124(2):483-488.
35. U.S. Food and Drug Administration, Center for Drug Evaluation and Research. EXPAREL NDA 022496 approval letter. October 28, 2011. http://www.accessdata.fda.gov/drugsatfda_docs/appletter/2011/022496s000ltr.pdf. Accessed January 2017.